About a third of the world’s population is chronically infected with the protozoan parasite Toxoplasma gondii. Data from the U.S. Centers for Disease Control and Prevention (CDC) suggest that about 11% of the U.S. population aged 6 years and over is infected with the parasite, while in other countries the infection rate has been shown to be up to 95%.
Researchers from 16 institutions across the U.S., Canada, England, Scotland, and Australia have now analyzed genetic, transcriptomic, and proteomic data from infected individuals, and from studies in cell cultures, to link T. gondii infection with a number of brain disorders, including epilepsy, Alzheimer’s and Parkinson’s diseases, and even some cancers. “This study is a paradigm shifter,” stated co-author Dennis Steindler, Ph.D., director of the Neuroscience and Aging Lab at the Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University. “We now have to insert infectious disease into the equation of neurodegenerative diseases, epilepsy, and neural cancers. At the same time, we have to translate aspects of this study into preventive treatments that include everything from drugs to diet to lifestyle, in order to delay disease onset and progression.”
Most people with a healthy immune system will develop no symptoms from infection with T. gondii. Individuals with compromised immune systems, however, are at risk from potentially far more serious complications of the infection that can affect the eyes, brain, and other organs. A pregnant mother who becomes infected can also pass the parasite to her unborn child, with severe, potentially fatal consequences.
Prior research has indicated that T. gondii infection in rodents and in primates can cause subtle behavior changes, including loss of the animals’ aversion to the smell of the urine of their natural predators. Some epidemiological studies in humans have linked T. gondii infection with neurological disorders such as Parkinson’s and Alzheimer’s diseases. However, this type of study can’t provide any information on gene networks in the human brain that are altered by the parasite, and which might provide insights into how to cure or prevent such diseases, Dr. Steindler and colleagues write in their published study in Scientific Reports, which is entitled “Toxoplasma Modulates Signature Pathways of Human Epilepsy, Neurodegeneration & Cancer.”
The researchers devised a set of studies that were designed to focus on the infectome—essentially “the human host and parasite molecules, and pathways that are perturbed by the interaction of the human host and parasite T. gondii”—to identify links between secreted parasite proteins, human microRNAs, neural chemistry, and pathways that are altered through host-parasite interactions.
“We wanted to understand how this parasite, which lives in the brain, might contribute to and shed light on the pathogenesis of brain diseases,” said Rima McLeod, M.D., professor of ophthalmology & visual science and pediatrics and medical director of the Toxoplasmosis Center at the University of Chicago. “We suspect it involves multiple factors. At the core is an alignment of characteristics of the parasite itself, the genes it expresses in the infected brain, susceptibility genes that could limit the host’s ability to prevent infection, and genes that control susceptibility to other diseases present in the human host. Other factors may include pregnancy, stress, additional infections, and a deficient microbiome. We hypothesized that when there is a confluence of these factors, disease may occur.”
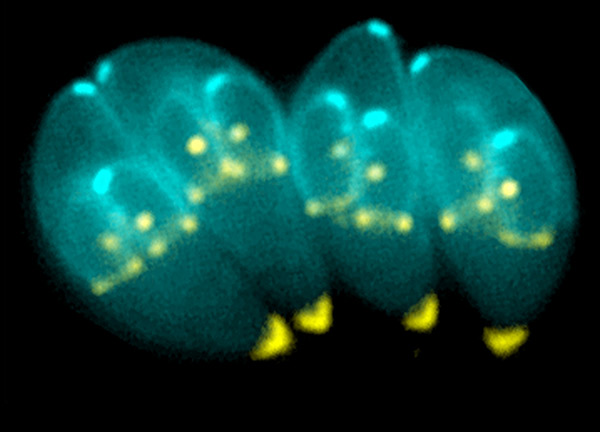
Using data from the National Collaborative Chicago-Based Congenital Toxoplasmosis Study (NCCCTS), which has followed 246 congenitally infected persons and their families since 1981, the researchers carried out what they called a “comprehensive systems analysis,” to identify parasite-related biomarkers and evaluate their potential impact. The team also looked at the effect of T. gondii infection in cultured primary neuronal stem cells, to evaluate gene expression and protein signatures. The study combined host genetics proteomics, transcriptomics, and circulating microRNA data to generate a model of how T. gondii affects the human brain.
The team then applied what they describe as a reconstruction and deconvolution approach to identify connections between T. gondii infection and altered pathways in neurodegenerative diseases, as well as connections between toxoplasmosis, human brain disorders, and some cancers. “Our results provide insights into mechanisms whereby this parasite could cause these associated diseases under some circumstances,” the authors wrote. “This work provides a systems roadmap to design medicines and vaccines to repair and prevent neuropathologic effects of T. gondii infection of the human brain. Furthermore, our original template provides a novel method to integrate multiple levels of intrinsic and extrinsic factors highlighting a way to unravel complexity in brain parasitism, toxoplasmosis specifically, and other complex diseases.”